I’ve always been interested in the idea of public health.
People have likened the idea of medicine in the developing world (or elsewhere) to pulling drowning people off of a raging river. Whereas, public health would be going upstream to figure out why so many people are falling into the river in the first place.
Of course, if all your time is spent saving the drowning, it’s pretty hard to find the time to pull yourself away to take a walk upstream. Important and necessary, but challenging to prioritize nonetheless.
After six years of serving as medical missionaries Burundi, a small country in Central Africa, my husband Eric and I decided to take that walk.
A Pattern Emerges
Ever since my first months serving as an OB-gyn at Kibuye Hope Hospital, I have noticed a huge amount of uterine rupture (UR) cases.
They are very rare in the US, but we have about 20 cases per year here in Burundi.
(***Side note for the medical folks: I looked at cases of uterine rupture from 2015-2017 and found 55, which is over 1% of our deliveries. !!?? Only about 50% of them are on uteri with previous scar. So, we have a huge amount of UR on unscarred uteri, which is pretty rare in the medical literature. Harder to prevent for sure.)
What could make a difference?
A big risk factor for uterine rupture is labor after a previous Cesarean section.
Everyone in the health community here “knows” this, but given broken systems and difficulty in education, many women who are at risk for UR continue to labor at home, in their villages, way after their due dates, instead of receiving a scheduled C-section or coming into the hospital to deliver under surveillance.
Some women show up with three previous C-sections, in labor, and don’t even know their due date.
If only we could find a way to get these ladies to come in sooner, to decide if a C-section is the best decision, and to choose a date for that C-section, maybe we could prevent some of these cases of UR. At the very least, we can decrease complication rates of infection, hemorrhage, fetal distress, etc, which are all higher in women with emergent vs scheduled C-sections.
Enter, Zigama Mama
Zigama Mama means “protect the mother” in Kirundi, the local language. Our Burundian friends say that’s not exactly the way they would say it…but we decided to use the phrase anyway given its catchy nature!
Our hospital is the referral site for 17 health centers in our district.
Any woman needing a C-section or increased surveillance would get sent from them to us, which also explains why our C-section rate is about 30% of our deliveries each year (instead of the national average of 6%).
The idea behind Zigama Mama was to look at all of our C-section data from the health centers for one year, then do a training session for the nurses at the health centers.
The intervention is simple: every woman with a previous C-section, even one, gets identified by the nurses, written into a register, and then she gets a coupon for a **free ultrasound** at Kibuye Hospital.
While ultrasounds are recommended in pregnancy, they are cash pay ($5) and most women can’t afford them.
So, the free ultrasound is the incentive to come to Kibuye, where I can confirm their due date and decide if a C-section is indicated or not.
If yes, I schedule it. If no, I encourage the women to come to the hospital (not the health center) for monitoring as soon as labor starts. That’s it.
We’ll look over the next year to see if our rates of emergent C-section and UR decrease.
The Response?
We had the initial training session last week. Honestly, I wasn’t sure how it was going to go. Eric made up a schedule that involved a start time of 8:30.
At 8:30 on Thursday morning, only one person (out of the possible 35) was there!
However, people trickled in over the next hour and in the end, 16 out of 17 health centers were represented!
We presented the rationale for the program, the nuts, and bolts, and then had several hours to do some training for the nurses on postpartum hemorrhage and neonatal resuscitation, as well as share a meal together in the canteen. It was great to see our Burundian doctors coming in to help out with the hands-on training programs.
Then, on Monday morning, I actually already had four ladies show up with their Zigama Mama coupons!
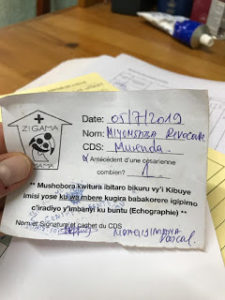
A Zigama Mama Coupon
I’m excited to see how this intervention can have a positive impact on the health of women in our district. There remain so many barriers to access to care, but hopefully, little by little, we can chip away at them.
———
The Serge team in Burundi currently needs more health professionals to work at the university or teaching hospital. Check out the specific staffing needs here. You can also start here to learn more about Serge’s medical missions work.
———
This post was originally published on www.mccropders.blogspot.com. Dr. Rachel McLaughlin gave Serge permission to share.